
Больница ALICANTE General Hospital — яркое место для уход за пациентом с инсультом в Валенцианском сообществе. Один из 23 инсульт центров в четвертом по численности населенном пункте Испании, до недавнего времени был единственным с время от поступления до введения препарата 30 минут.
Это не было совпадением. Больница также была единственной в регионе, где в плановом порядке регистрировали и анализировали данные о лечение, терапия инсульт, и пример того, как мониторинг качества влияет на практику.
Но здесь и Covid оставила свой знак. На высоте пандемии инсультное отделение в больнице общего профиля Аликанте превратилось в отделение интенсивной терапии. Как и в некоторых других инсульт отделениях, которые исчезли под давлением другого набора приоритетов, он все еще не восстановил свой статус специализированной палаты, где пациенты с инсульт получают наиболее подходящую медицинскую помощь от многопрофильной группы специалистов.
Это был только один из вопросов, который занимал мысли неврологов со всего Валенциевого сообщества, которые посетили ориентирное совещание 16 июня. Принимая во внимание острую потребность в стандартизированном уход за пациентом с инсультом в регионе, консультант Angels Белен Веласкез собрал организационный комитет, состоящий из главных неврологов из шести валенциальных больниц — по две из провинций Кастельон, Валенсия и Аликанте. Также присутствовали представители двух теле- инсультных больниц, координаторы С помощью СМП по каждой провинции, региональный директор С помощью СМП Бегоня Аргос и Кристина Руиз Каванильцы из Валенцианского департамента здравоохранения.
Присоединились к встрече из Барселоны: д-р Наталья Перез де ла Осса и Ксавьер Хименес, соответственно, директор Каталонии по инсульт и медицинский директор С помощью СМП, которые пришли поделиться своими идеями о планировании и организации со своими соседями. В повестке дня были высоки показатели коммуникации, а также важность мониторинга качества и приоритетные меры по устранению задержек лечение, терапия.
Программа мониторинга качества, реализуемая в пяти больницах два года назад, нарисовала мрачную картину, демонстрируя среднее время от поступления до лечение, терапия, значительно выходящее за рамки рекомендаций. Числа указывали на желание многопрофильной командной работы внутри больниц и отсутствие координации между больницами и между больницами и С помощью СМП, при этом код инсульт был активирован всего в 45% случаев.
Географически почти 5 миллионов жителей Валенсийского Сообщества хорошо обслуживаются тремя (вместе четыре) комплексными центрами и 20 репрезентативными больницами. Однако для получения наилучшего лечения необходимо совместное принятие мер по стандартизации, улучшению, основанному на данных, и оптимизации маршрута для пациентов с инсульт в регионе. Именно в этом будет состояться эта встреча.
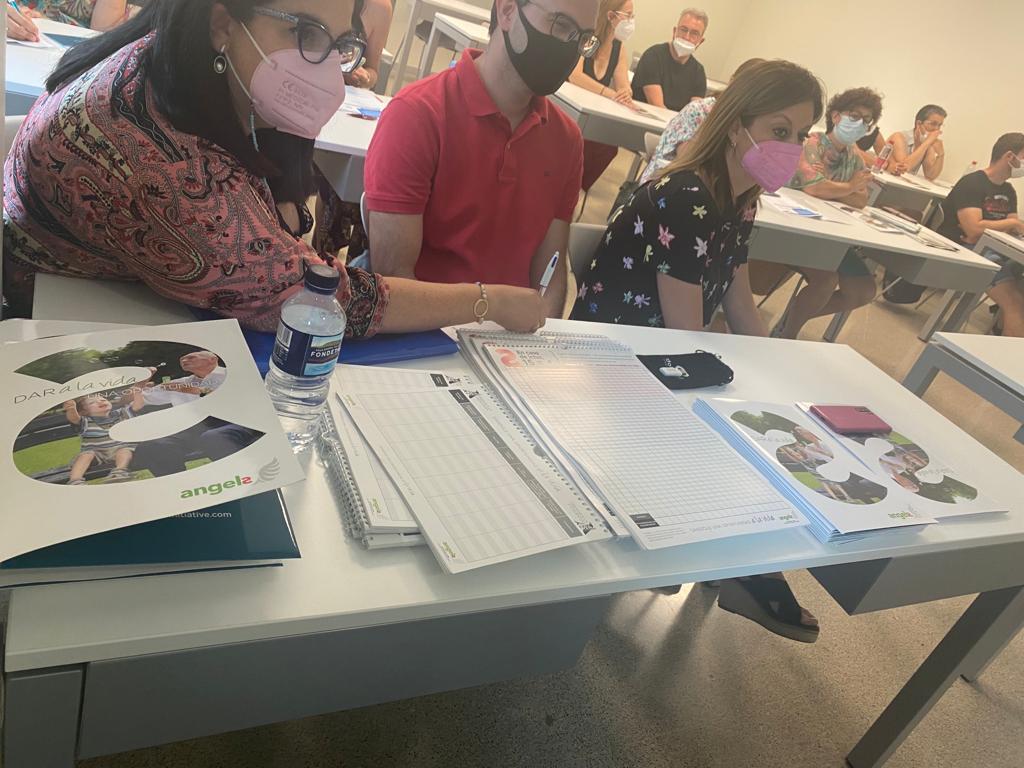
ЭЛЕВЕН ДНЕЙ позже 27 июня Белен назначит 20 медсестрам из Кастельона, Валенсии и Аликанте домашнее задание. Руководители медсестер и медсестры инсульт отделений из шести больниц в Валенсийском сообществе присутствовали на первой встрече организационного комитета медсестер, которая в ближайшие месяцы рассмотрит необходимость стандартизированного протокола уход за больными ухода при инсульт и обучения в регионе.
Теперь им назначена задача на лето. Каждая команда медсестер должна пересмотреть свои сильные стороны и определить области уход за больными пациентами с инсульт, в которых они обладают специальными знаниями и опытом. Когда дело доходит до составления протокола ухода после обострения в Валенсии, медсестры из каждой больницы будут вносить вклад в получение знаний из области, в которой они являются экспертами.
Медсестры в Валенсийском сообществе сталкиваются с уникальным набором препятствий. Регион имеет самое низкое соотношение медсестра и пациент в стране, что создает проблемы в инсультное отделение, как это делает в других странах. Но хотя встреча согласна с важностью сообщения об этом органам здравоохранения, сегодняшняя задача — оптимизация имеющихся у них ресурсов. Кроме того, что они объединят свои знания и опыт в составлении протокола инсульт, они будут сотрудничать в обучении и совместно принимать участие в Хельсинкской задаче, чтобы оценить свой прогресс. Это был только вопрос часов, но уже это сообщество, которое вместе сильнее и играет в свои сильные стороны.

ОБУЧЕНИЕ также входит в число целей, согласованных на совещании больниц и служб С помощью СМП 16 июня. Провинция будет проходить по провинции, начиная с многопрофильных встреч, и все шесть больниц будут проводить моделирование маршрута с использованием С помощью СМП.
Реестр был выбран. В будущем данные о лечение, терапия из разных регионов будут регистрироваться в RES-Q, а выводы, полученные в результате анализа, будут использоваться для определения возможностей улучшения.
Летний перерыв в сентябре 2022 г. покажет момент, когда Вальянское сообщество официально вступит в новую главу по уход за пациентом с инсультом. Но хотя бы одна больница не готова подождать.
Через один день после заседания организационного комитета медсестер обучение в инсультное отделение начинается в больнице La Fe de Valencia. В пользу того, что на собрании в город были приглашены как Angels, так и эксперты по инсульт, медсестры этой больницы посещают учебный курс, который включает обзор протокола инсульт, введение в Пройэкто Флеча (вмешательство на Малаге для устранения вариабельности в уходе после обострения) и общение с семьями пациентов при выписка.
Гальванизированные совещанием предыдущего дня, они решили, что сейчас было такое же время, как и любое, чтобы повысить стандартное лечение в своем отделении. В конце концов, когда речь идет об инсульт, буквально ничего не имеет значения больше, чем время.




